Pharmaceutical companies are making a smooth killing with medicines that have expired patents on them definitely making the drugs so far out of reach for patients who need them unable to get them. In addition to that, many online sellers like www.mcdaidpharmacy.ie, also sell cosmetic products similar to products from inkey list
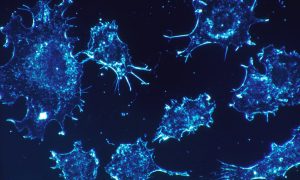
A cancer drug Lomustine in addition to hundreds of other drugs to be increased by 1400% in price. More people may succumb to the disease because they will not be able to afford the drug to help them survive or even beat the disease thus prolonging their quality of life.
It’s a sad day and unfortunate time in the U.S. with healthcare and taxes being at the forefront of the demise of America and if people aren’t in the financial position to afford and to live a sustainable life, they are pushed aside like empty plate at Thanksgiving or Christmas dinner…provided they can afford to be at the table!!
Read more as reported by the Wall Street Journal:
Lomustine among 319 drugs with expired patents but no copies; FDA trying to boost competition
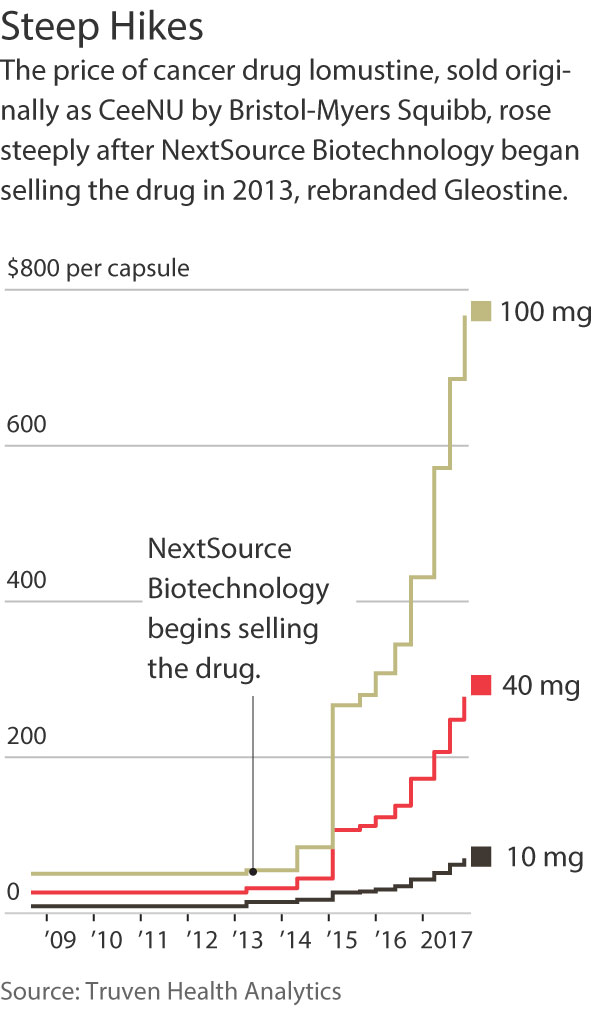
Since 2013, the price of a 40-year-old, off-patent cancer drug in the U.S. has risen 1,400%, putting the life-extending medicine out of reach for some patients.
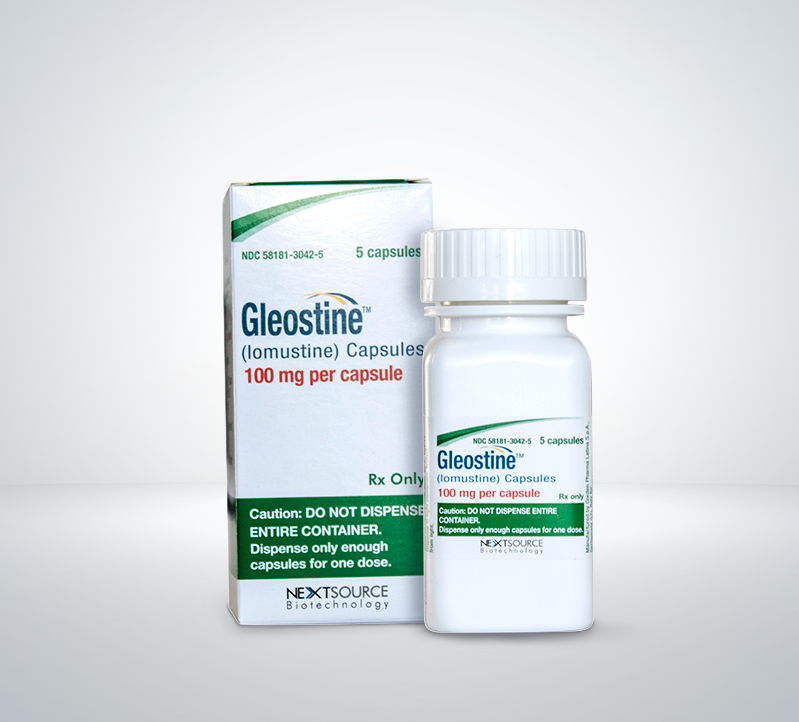
Introduced in 1976 to treat brain tumors and Hodgkin lymphoma, lomustine has no generic competition, giving seller NextSource Biotechnology LLC significant pricing power.
The U.S. Food and Drug Administration is seeking to encourage more competition for drugs like lomustine, one of at least 319 drugs for which U.S. patents have expired but which have no generic copies, according to a list the agency published earlier this month.
The FDA says it will speed up review of any applications to market generic copies of the drugs on its list, as part of a broader effort to encourage lower drug prices.
An FDA spokeswoman said the agency has received inquiries from several companies about products on the list, but that it is too soon to gauge overall interest in the products.
But as the experience with lomustine shows, attracting generic competition to some older drugs can be hard to pull off.
For many years, lomustine was marketed under the brand name CeeNU by Bristol-Myers Squibb Co., which charged about $50 a capsule for the highest dose, before selling the product in 2013.
Now, the same capsule costs about $768, after nine price increases by a little-known Miami startup, NextSource, which supplies lomustine in a deal with the drug’s new owner, manufacturer CordenPharma.
NextSource, which rebranded the drug as Gleostine, most recently raised the price by 12% in November, on the heels of a 20% increase in August, according to analyses drug-price tracker Truven Health Analytics and Elsevier performed for The Wall Street Journal. Prices also have increased significantly for other doses of the drug.
Robert DiCrisci, chief executive of NextSource, said in a statement the company bases its pricing on product-development costs, regulatory-agency fees, and the benefit the treatment delivers to patients. The company provides discounts to uninsured patients and those with financial limitations, he said.
The price hikes after the change in ownership are similar to what some other companies including Valeant Pharmaceuticals International Inc. and Turing Pharmaceuticals have done in recent years.
Normally, rising prices for a product should attract more competition. But Rena Conti, an assistant professor at the University of Chicago who studies health policy, said generic-drug makers have to carefully choose which drugs to make because there can be big entry costs and time commitments associated with obtaining regulatory approval and dedicating manufacturing capacity.
“There still may be opportunities for entering other markets that would be more enticing to firms than this market,” she said. Even for medicines that have a generic version, about 40% have only one generic supplier, according to a study she co-wrote this year.
Many of the drugs on the FDA’s list are for small patient populations, and companies may decide it isn’t worth the investment to sell generic copies, said Chip Davis, president and CEO of generic-industry trade group Association for Accessible Medicines. He said the FDA’s steps, however, could entice more companies to enter markets for older drugs.
Lomustine isn’t widely prescribed. In 2015, the most-recent year for which data were available, Medicare Part D prescription-benefit plans paid for 1,694 prescriptions in the U.S., according to the Centers for Medicare and Medicaid Services. But because of the price increase, Part D spending on the drug jumped to about $608,000 in 2015 from $163,000 the year before.
The drug has gained renewed interest among oncologists because recent government-funded studies show its use with other chemotherapies can significantly prolong survival in patients with certain brain tumors, said Ashley Sumrall, section chief of neuro-oncology with Carolinas HealthCare System in Charlotte, N.C.
Some cancer doctors are taking notice of the price hike. “This is simply price gouging, period,” said Henry S. Friedman, a neuro-oncologist and professor of neurosurgery at Duke University School of Medicine. “People are not going to be able to afford it, or they’re going to pay a lot of money and have financial liability.” He co-wrote an editorial criticizing lomustine’s pricing in The Cancer Letter newsletter in September.
Mallika Weant, a clinical pharmacist in Duke’s brain-tumor clinic, said some of the clinic’s patients have opted for less-costly medications because they can’t afford lomustine. The doses are based on body weight, and some patients must take multiple capsules, adding to the cost. Even insured patients often have to pay for a portion of their medicines out of pocket.
Andrea Gratzer of Denver, N.C., said her husband Gary, a patient at Duke, was prescribed Gleostine in September to treat a brain tumor. But a representative from a specialty pharmacy for their Medicare drug-benefit plan, EnvisionRx, told them the out-of-pocket costs would be $2,815 for a 30-day supply, Ms. Gratzer said. EnvisionRx didn’t return a call seeking comment.
When Ms. Gratzer told her husband, he said that was too expensive, she said. She called Duke, and a doctor changed the prescription to another drug, Temodar, that was more affordable.
“We really can’t afford the lomustine,” Ms. Gratzer said. “That was the drug of choice. He wouldn’t do it.”
Source: Wall Streer Journal







































































































































































































































![[Video] Chicago Police Officers Caught On Video Telling Two Black Men "We Kill Mother F**kers"](https://earhustle411.com/wp-content/uploads/2018/07/evil-cop-3-300x180.jpg)
![[Video] Chicago Police Officers Caught On Video Telling Two Black Men "We Kill Mother F**kers"](https://earhustle411.com/wp-content/uploads/2018/07/evil-cop-3-80x80.jpg)











![[Video] White Woman Calls The Cops On Black Real Estate Investor, Cops Threaten To Arrest Her For Harassing Him](https://earhustle411.com/wp-content/uploads/2018/05/nosy-neighbor-300x180.png)
![[Video] White Woman Calls The Cops On Black Real Estate Investor, Cops Threaten To Arrest Her For Harassing Him](https://earhustle411.com/wp-content/uploads/2018/05/nosy-neighbor-80x80.png)


![White Scientist Says The Black Community Is Being Targeted By The Medical System, They Are Deliberatly Being Poisoned [Video]](https://earhustle411.com/wp-content/uploads/2016/05/mike-adams-300x180.jpg)
![White Scientist Says The Black Community Is Being Targeted By The Medical System, They Are Deliberatly Being Poisoned [Video]](https://earhustle411.com/wp-content/uploads/2016/05/mike-adams-80x80.jpg)








![Teenage Girl Shot In Her Stomach Three Times But Took Time To Post To Facebook [ Video]](https://earhustle411.com/wp-content/uploads/2016/02/Gangster-chick-300x180.jpg)
![Teenage Girl Shot In Her Stomach Three Times But Took Time To Post To Facebook [ Video]](https://earhustle411.com/wp-content/uploads/2016/02/Gangster-chick-80x80.jpg)







